CMSPricer provides a significant value in increasing first pass through rate for claims when working the revenue cycle. This has become increasing difficult due to coding complexities, changing CMS rules, and regulatory changes. These rules and regulations also continue to change every single day. Due to these changes and regulations, it’s imperative to have an automated method to validate your claims before they are generated and submitted to payers so you can avoid downstream denials and delayed payments like the CMSPricer editing solution which is fully automated via API.
What do these edits entail?
How this helps our clients:
Results of using CMSPricer edits include:
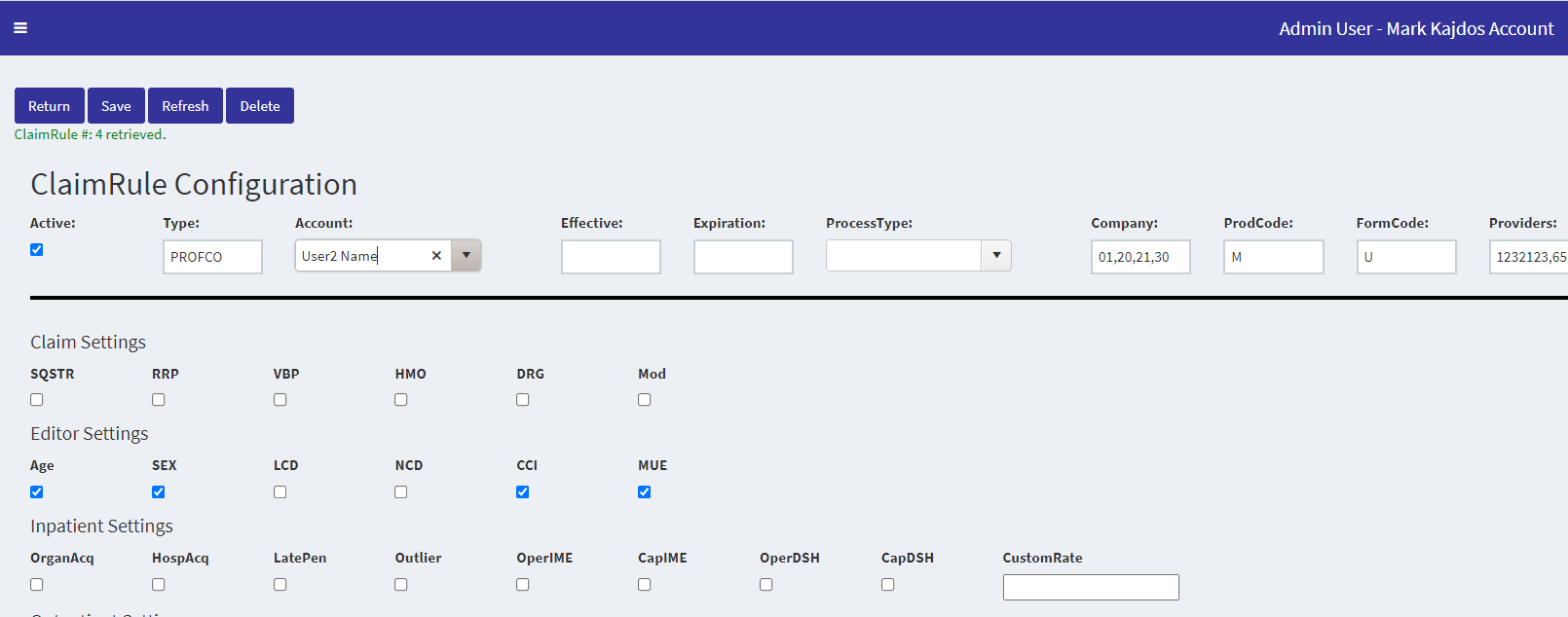
Step 1 - Simply configure the edits “on/off” and CMSPricer will edit the claim accordingly. We also have clients that run an API for easy and automatic feeds back into your process workflows.